CARE NAVIGATION WITH CLINICAL EXPERTISE
The perfect balance of high-touch, clinical, and cost-effective support.
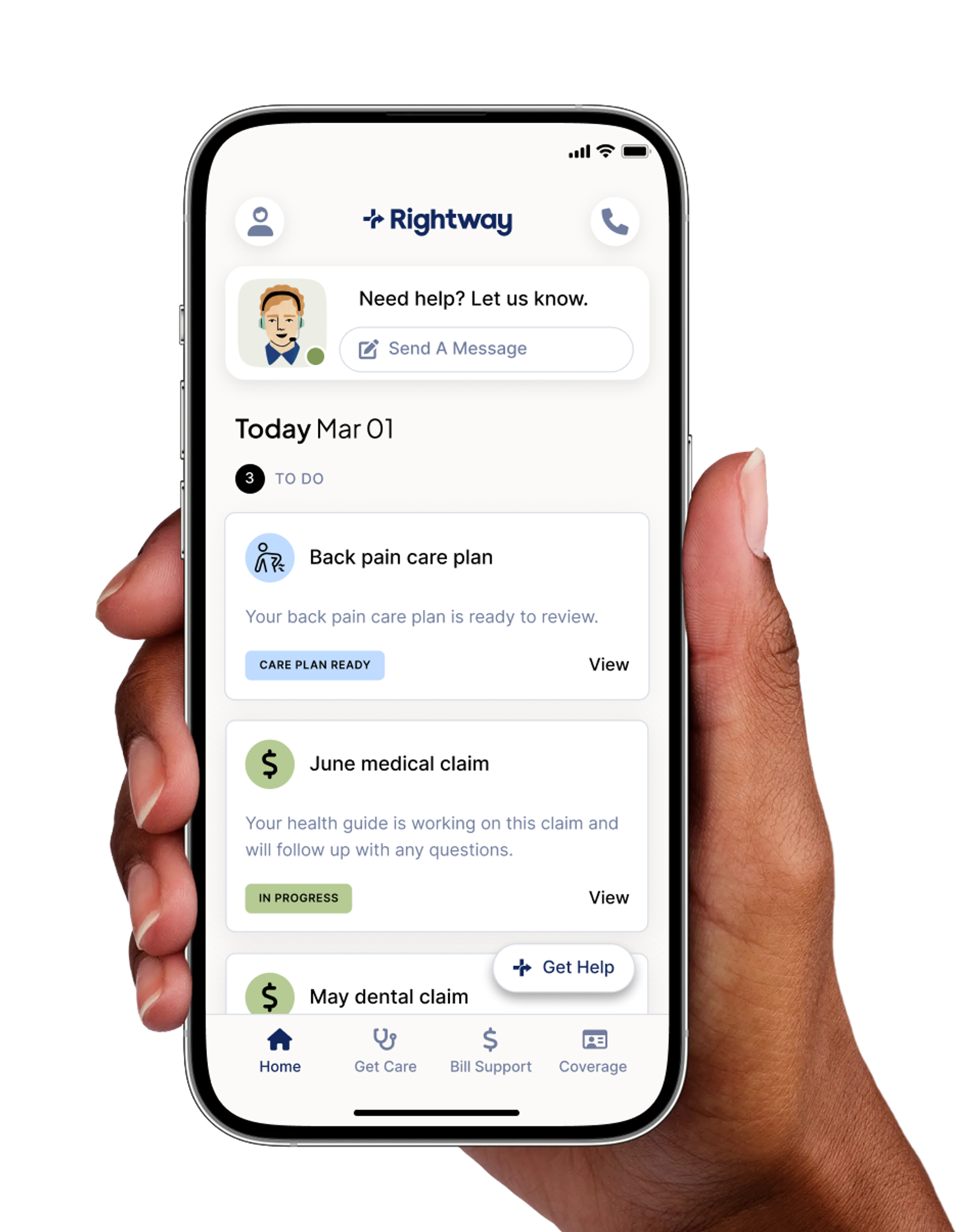
Rightway makes it simple for your employees to navigate their healthcare and get the most from the benefits you already offer.
Whether that means finding the right doctor, understanding their coverage, resolving a billing issue, or getting quick answers from a trusted expert—Rightway care navigation combines expert nurse-led guidance with smart technology to support your people.

Other care navigation solutions don’t solve much.
Most care navigation solutions are either outrageously expensive, outdated, or outsourced to call centers that leave members so frustrated that they’d rather find their way through healthcare on their own. For so-called solutions, they really don’t solve much.

We don't just wait for problems.
Real care means reaching out first.
We take a proactive approach to support that helps keep your members engaged, healthy, and equipped to make the most from their benefits. We help them stay on top of their health, preventing unexpected costs along the way.
Our in-depth support helps
benefit teams do more with less.
We deliver unmatched member support, including handling tasks on their behalf, so your team isn’t stuck solving benefits issues. We keep your employees healthy and cared for, freeing you up to focus on what matters most. All support is part of your Rightway benefits, with no pass-through to your employees.
we support employers with:
Personalized strategies that activate and engage employees. We know how to help your members take action.
Full-stack benefits support on everything from coverage questions to bill resolution. Nothing is off limits.
Seamless coordination with third-party programs, with requirements, workflows, and points of contact defined upfront to ensure a smooth integration.
Predictive analytics that identify at-risk members and close care gaps. We get ahead of issues before they happen.
Well-managed, high-touch implementation that makes transition a breeze. Our team does the heavy lifting, so yours barely has to lift a finger.
Proven methods to reduce costs by addressing care gaps, minimizing ER visits, and improving access to high-quality, affordable care.
We focus on the metrics that matter.
We make healthcare work for your members and save you money. And we’ve got the data to prove it works.
See our care navigation in action.

We don’t just promise to save you money. We guarantee it.
Our care navigation model is proven to reduce healthcare spend by 15%, and we guarantee a 2x ROI in year one. We stand by our approach because we know it works, and because you and your people deserve a benefits partner who takes accountability.
WHEN CARE NAVIGATION IS PAIRED WITH PBM
A unified healthcare and pharmacy experience.
Rightway’s care navigation is strengthened when combined with our pharmacy benefits management (PBM) solution. Rightway nurses, health guides, social workers, and billing specialists are supported by our pharmacy team to support members throughout their healthcare journey.
With unified insights across medical and pharmacy data, this collaborative team resolves medication barriers, supports therapy optimization, and proactively guides members at critical moments in their care.


“Rightway helped us reduce our total healthcare spend by 5% and non-catastrophic spend by 9%, while engaging 62% of our employees in the first year.”
Trusted by leading organizations
Employees are more productive when their healthcare needs are met. So are their benefits leaders.
