Welcome to a better pharmacy benefit experience.
Roche has partnered with Rightway to manage your pharmacy benefits.
With Rightway, you and your covered dependents have access to tools and support that will help you save time and money on your prescriptions.

Rightway is the new pharmacy benefit manager (PBM) for Roche employees and family members enrolled in UnitedHealthcare medical plans.
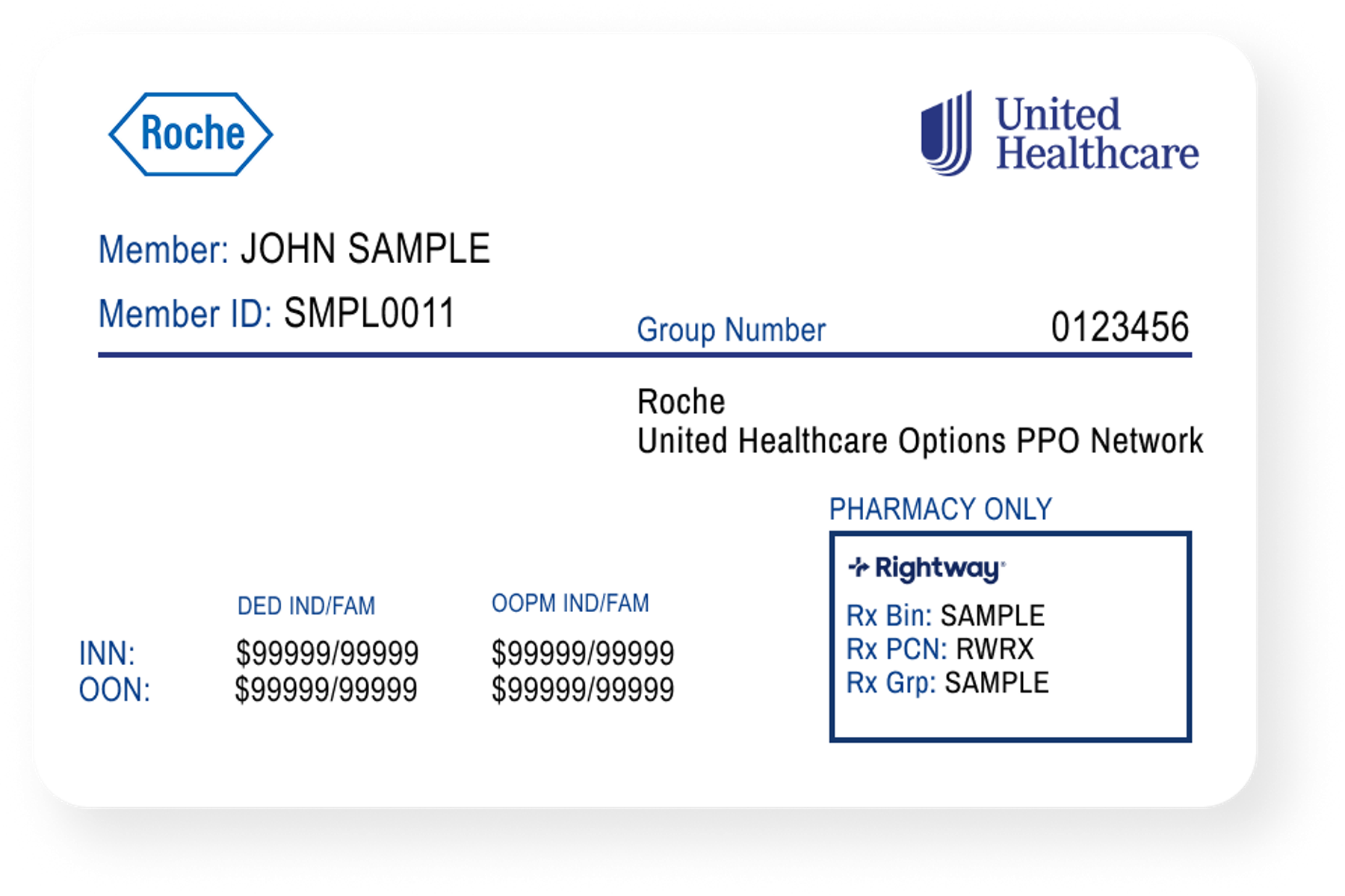
Be sure to use your new UnitedHealthcare ID card when you pick up a prescription at a pharmacy.
Easily see if your medication is covered.
Find out if your medical plan covers your medication by:
- Typing the drug name into the search box.
- Using the A-Z list to search by the first letter of the drug name.
- Browsing by therapeutic drug class of the medication.

Mail-order pharmacy services.
Rightway partners with Walgreens Mail Service and Mark Cuban Cost Plus Drugs to deliver prescriptions to your home, helping you save time and money. Contact our pharmacy team if you need help choosing the best option or transferring a prescription to your preferred mail-order pharmacy.

Please note that Walgreens Mail Service does not offer pickup at Walgreens retail pharmacy locations.
Resources:

Learn about Cost Plus Drugs’ services and how to get started.
Resources:
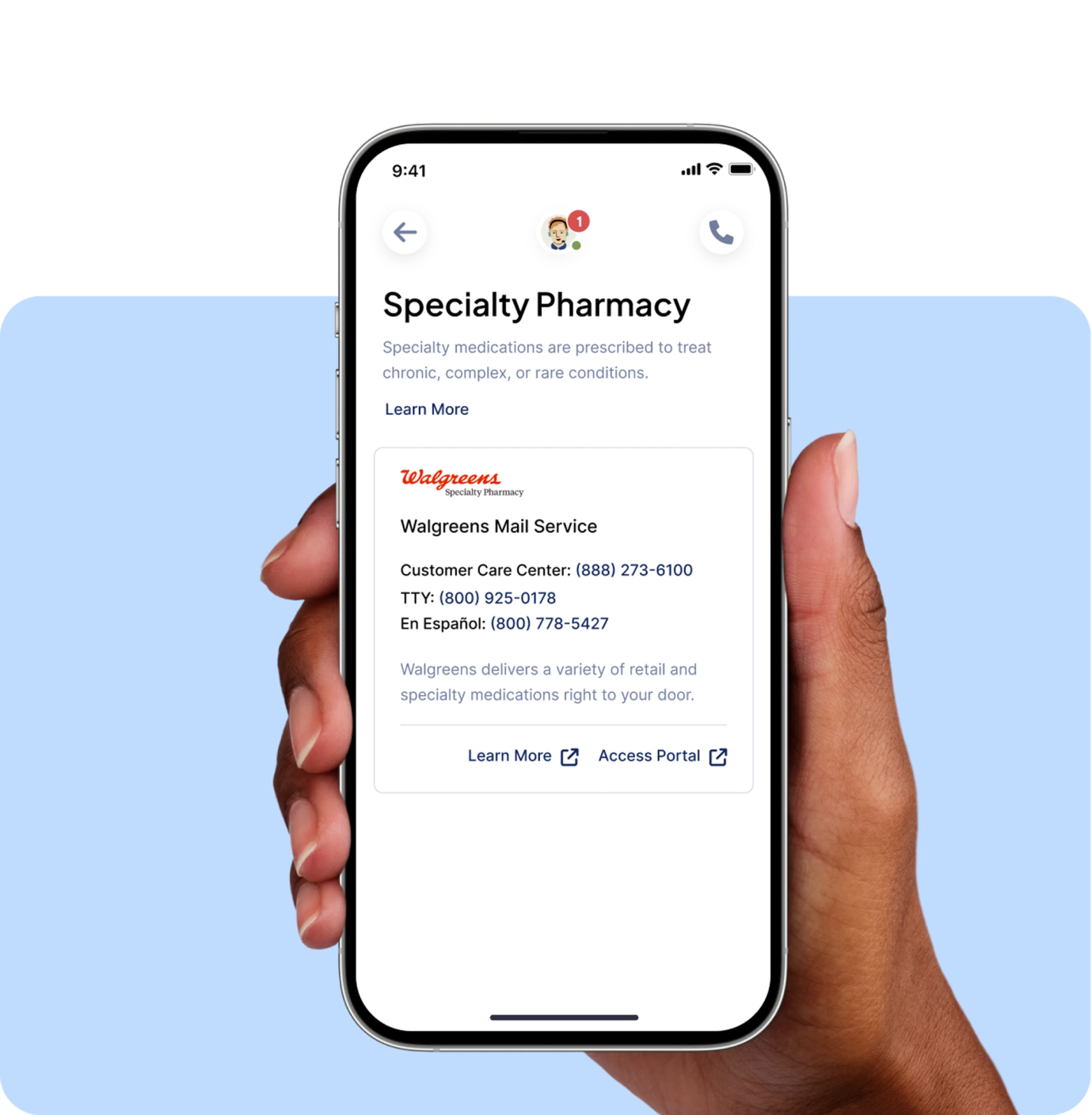
Specialty pharmacy services.
Rightway partners with several specialty pharmacies to deliver specialty medications right to your door. Our specialty pharmacy team is here to guide you through the process and ensure you get your prescription when you need it.
To order a specialty medication, follow the steps below or reach out to us at 833-419-8391.
Authorization.
Confirm that your provider has obtained prior authorization from Rightway for your specialty medication. We're happy to contact your provider to start this process.
Once approved, your provider will be directed to send your prescription to one of Rightway’s specialty pharmacy partners.
Registration.
Register with the specialty pharmacy and enroll in copay assistance programs (if available).
Once your registration is complete, the pharmacy will fill your prescription and ship it to you.

Communication.
Use your specialty pharmacy account to schedule refills and check the status of your order. If you have any trouble accessing your medication, reach out to Rightway for assistance.
Access forms and
important documents.


Not seeing a document you need?
Frequently asked questions.
Can I continue to fill prescriptions at my current pharmacy?
In most cases, you can continue to fill prescriptions at your current pharmacy; Rightway’s pharmacy network includes many local and national retailers, including CVS, Rite Aid, Walgreens, and Walmart.
Be sure to use your new UnitedHealthcare ID card whenever you pick up a prescription. (If you haven’t received your new ID card, please contact the UnitedHealthcare Health Team at 888-264-0749.) You can also access your ID card through the Rightway app Apple App Store/Google Play and myuhc.com.
My pharmacy couldn’t fill my prescription. What happened?
Your pharmacy may not have been able to fill your prescription because it doesn’t have your new coverage information. Ask the pharmacy to try to fill the prescription again using the information on your new UnitedHealthcare ID. If you don’t have your new ID card with you, you can pull it up on the Rightway app Apple App Store/Google Play or reach out to our Rightway pharmacy team for help.
How can I tell if my local pharmacy is in the Rightway network?
You can use the Rightway app Apple App Store/Google Play to see which of your local pharmacies are in the Rightway network. You can also use the app to compare medication costs at different pharmacies (and fill your prescription at the one that offers you the best balance of cost and convenience). If you need finding a network pharmacy, reach out to our Rightway pharmacy team.
Will my medications continue to be covered?
A “formulary” is a list of medications covered under a prescription drug plan. The medications that were included on the Optum Rx formulary are included on Rightway’s formulary. We expect to make some changes to our formulary for 2026, and will provide more information in early October.
Have a question? Contact your pharmacy team.
Rightway is here to help answer questions and take action for you.