PBM reform update: What employers must know about CAA 2026 and DOL PBM disclosure rule.

Rising prescription drug costs and heightened fiduciary scrutiny have placed PBM arrangements under increased focus. For many years, legacy pharmacy benefit manager(PBM) structures have relied on opaque pricing mechanisms that limited employer insight and made it challenging to evaluate alignment between PBM incentives, employer interests, and member outcomes. Recent federal action reflects a clear policy intent to modernize PBM oversight and move the market toward transparent, value-driven, client-aligned models.
Rightway was built to solve these problems. Our model doesn’t respond to regulatory pressure—it defines the standard these reforms are working toward. Transparency, client alignment, and simplicity aren’t add-ons or adjustments for us. They are part of our foundation.
Rightway is already positioned for compliance as regulatory expectations evolve. That said, these reforms matter—not because they change how we operate, but because they signal where the market is headed and provide a useful framework for evaluating PBM partnerships. Here’s what you should know.
CAA 2026: Enacted PBM reform.
The Consolidated Appropriations Act, 2026(CAA 2026) establishes comprehensive, statutory PBM reform requirements that will apply to most employer-sponsored group health plans beginning with plan years starting 30 months after February 3, 2026 (January 1, 2029, for calendar-year plans). Key provisions include expanded PBM reporting, enhanced contract protections, and stronger audit rights. For large self-funded employers, PBMs will be required to provide detailed drug-level reporting, while all group health plans will receive plan-level summary reporting designed to improve visibility into prescription drug spend and PBM compensation.
For ERISA plans, CAA 2026 further reinforces transparency by requiring 100% pass-through of rebates and other remuneration, expanded compensation disclosures, and annual audit rights. These changes signal a meaningful departure from legacy PBM models and elevate transparency from a contractual preference to a statutory expectation.
DOL PBM disclosure rule as proposed.
In parallel with CAA 2026, the Department of Labor (DOL) has issued proposed regulations that would significantly expand ERISA disclosure requirements for PBMs and certain affiliated service providers. If finalized, the rule would require more frequent and detailed disclosure of direct and indirect PBM compensation, pricing methodologies, and incentive structures.
Although the proposed rule is not yet final, it reinforces the broader regulatory trajectory toward standardized, meaningful PBM transparency. Together, CAA 2026 and the DOL proposal provide a clear signal that opaque PBM structures are increasingly misaligned with regulatory and employer expectations.
While timelines can change, after the 60-day comment period closes, the DOL will provide comments/revisions. The proposed rule could become finalized in late 2026 or early 2027.
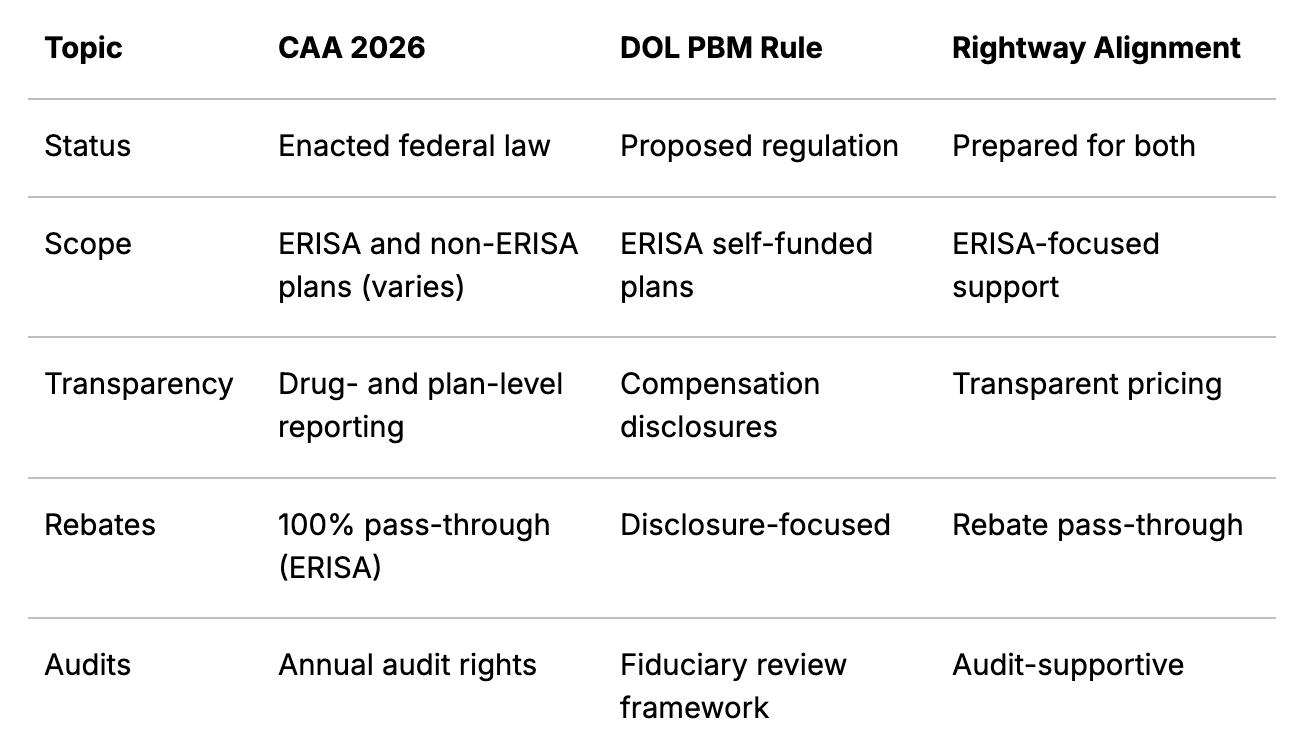
Comparing the two frameworks.
What this means for employers.
These reforms create a clear framework for evaluating PBM partnerships. Employers may want to assess:
- Whether PBM pricing structures are straightforward and clearly understood
- Access to timely, actionable prescription drug and rebate data
- Alignment between PBM incentives, plan objectives, and member outcomes
- Contract terms that support data access, audit rights, and flexibility as requirements evolve
Rightway supports this assessment with built-in transparency: no spread pricing, 100% rebate pass-through, and clear data access that doesn’t require regulatory enforcement to deliver.
Looking ahead.
CAA 2026 and the DOL’s proposed regulations reflect a broader shift toward PBM models that work for employers and members, not around them. Rightway was founded on this principle—not as a reaction to regulation but as a structural commitment to how we believe this industry should operate.
As these requirements take effect, Rightway will continue monitoring developments and sharing updates. Our approach remains consistent: transparency as a foundation, not a compliance checkbox.
Disclaimer: This communication is provided for informational purposes only and does not constitute legal advice. Employers should consult with legal or compliance advisors regarding their specific obligations under applicable law.







