The PBM designed for employers
Our neutral PBM is better for your members and your budget.
Unlike other PBMs, we don’t have conflict-of-interest relationships, so you can trust us to get your people the prescriptions they need at the lowest possible costs. Pharmacists at the center of our PBM means unmatched service for your team, and peace-of-mind for you.

Today’s PBMs have lost the plot.
Originally created to lower prescription costs, legacy PBMs are under fire for doing the exact opposite. They own undisclosed parts of the supply chain, inflate costs, and use rebates to create artificial savings. In other words, they give you the illusion of saving, while really increasing your total drug spend.
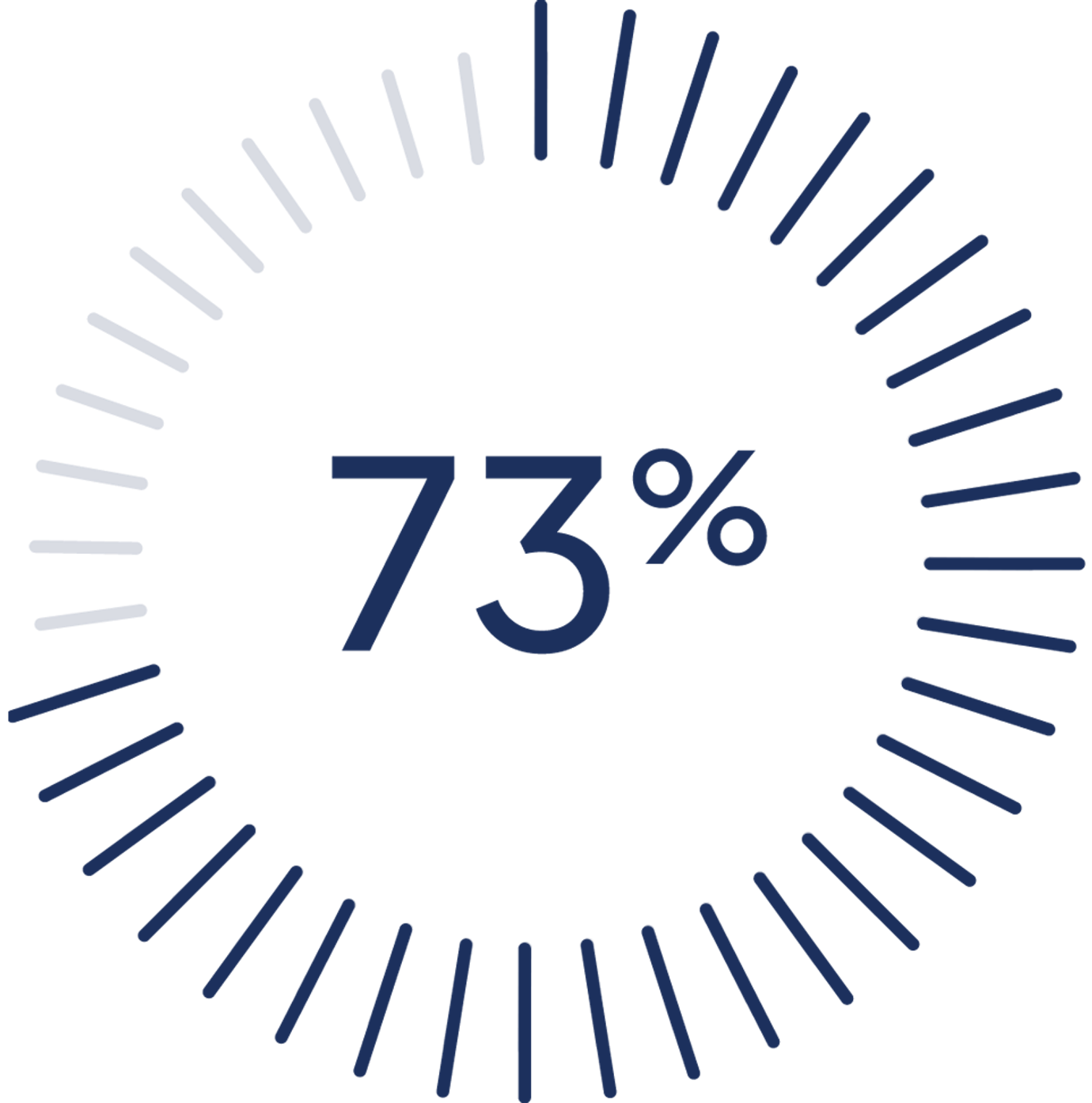
Of employers do not find their PBM to be trustworthy.

4 out of 5
Plan sponsors are dissatisfied with traditional PBM contracts.
“The big 3 PBMs are charging enormous markups on dozens of lifesaving drugs.” Hannah Garden-MonheitFTC Director of Policy Planning

A true benefits partner
It’s not enough to be transparent. That’s why we’re a neutral PBM.
Being neutral puts us on your side. We own 0% of the supply chain (unlike our competitors), have an entirely transparent pricing model, and pass back every penny we save to you and your members.
“I haven’t always been a fan of PBMs, but Rightway has truly delivered. They’ve helped our members save money, which is the ultimate goal, and reduced our claims costs. They’ve made a real difference for our members.”Mark SchaerrerVice President of Human Resources

We focus on the metrics that matter.
Rather than focusing on rebates, our model prioritizes overall spend and member service. And we have the data to prove it works.
What we offer.
PHARMACY EXPERTISE
The best member experience. Period.
We’re the only PBM with pharmacy navigation. Our team of licensed pharmacists is uniquely qualified to support your members, handle time-consuming tasks, like switching to mail order or activating cost-savings programs, and remove frustration across the entire prescription process.
REAL SAVINGS
A FULLY-SUPPORTED MEMBER EXPERIENCE
EXCEPTIONAL SERVICE FOR YOU
The only PBM with pharmacy navigation.
Centered around members, powered by pharmacists.
100% pharmacist-led support.
Every service interaction is handled by licensed pharmacists or pharmacy technicians who deliver clinical expertise.
Concierge clinical support.
Pharmacists answer medication questions, recommend lower-cost alternatives, coordinate mail-order transfers, and resolve pharmacy issues.
Trained to treat your people like you do.
Our clinicians are trained on each client’s demographics, culture, and benefits—functioning as a seamless extension of your benefits team.
Switching to Rightway is seriously simple.
We deliver a hands-on, well-managed implementation for you and your members. Clients consistently tell us that our proven playbook makes it easy to use Rightway on day one, and every day after that.

For employers.
We map out a detailed project plan, tailored to your goals and designed to minimize noise from your workforce.
Our entire team is certified in change management. They have the expertise to ensure a well-managed transition with clear communication and hands-on guidance.
Rightway handles the heavy lifting, like securing the data files from your carrier. Our modern infrastructure enables data transfer in hours, not weeks.
Your dedicated customer support team stays with you before, during, and after implementation to make sure we continue to meet goals.

For members.
Our robust member materials ensure your people get the right info: personalized, clear, and easy to act on.
An early app experience lets members explore their benefits before going live.
Our team proactively reaches out by phone, email, and mail—doing the work behind the scenes so members who need extra help feel cared for, confident, and never overwhelmed.
And for members who don’t, our app puts the power in their hands, helping them manage pharmacy benefits for themselves and their families.
Pay one fee per member
per month. That’s it.
Our pricing model really is that simple. We calculate a single, guaranteed per member per month (PMPM) administrative fee, and pass all savings back to you. Some PBMs claim they’re transparent. We actually are.
Rightway delivers cost control and accountability through:
100% transparency and pass-through pricing. Every claim is fully auditable, eliminating hidden fees, spread pricing, and rebate games that inflate total spend.
Pharmacist-led member guidance. Our pharmacy team directs members to lower-cost, clinically sound options—like generics and independent biosimilars.
Formularies built for savings. We select drugs based on the best clinical value, not the biggest rebate—preserving clinical integrity while cutting unnecessary expenses.
No ownership across the supply chain. We don’t own mail, retail, or specialty pharmacies—or any part of the supply chain—so recommendations always favor the plan’s bottom line, not ours.
The industry’s leading PMPM guarantee. A single, predictable monthly rate covers total pharmacy spend, with full year-end reconciliation for unmatched cost accountability.
Aligned incentives. Our model ties all fees and performance metrics to total plan spend and member satisfaction. We only succeed when you do.

“Each area of implementation was handled with the utmost care and consideration.”Renu ChhabraVice President and Head of Global Benefits & Total Rewards, Tyson Foods
WHEN PBM IS PAIRED WITH CARE NAVIGATION
A unified pharmacy and healthcare experience.
Rightway’s PBM becomes even more effective when paired with care navigation. Rightway’s pharmacy team works hand-in-hand with our nurses, health guides, social workers, and billing specialists to support members across their healthcare journey.
Through shared medical and pharmacy data, this collaborative team closes care gaps, delivers timely guidance, and intervenes at key moments—including new diagnoses, missed follow-ups, or adherence concerns.


“Rightway has delivered on their promise 100%. I’ve been doing this for 18 years and I’ve never had such good results from anyone in the health industry.”
Trusted by leading organizations
Employees are more productive when their healthcare needs are met. So are their benefits leaders.

ALBUTEROL
Save on your medication by transferring to a mail-order pharmacy.






