Rightway makes it easy to access specialty medications.
Rightway partners with trusted specialty pharmacies to deliver high-quality medications right to your door. Our specialty pharmacy team is here to guide you through the process and ensure you get your prescription when you need it.

Get started in 3 easy steps.
Rightway's specialty pharmacy partners help you manage your specialty medication therapy. If you have questions or need support, contact our specialty pharmacy team.
Confirm that your prescription is authorized.
Ensure your provider has secured prior authorization for your specialty medication. Rightway can also manage this process on your behalf. Then, your provider will send your prescription to the specialty pharmacy.
Set up your account.
Register with the specialty pharmacy, and enroll in copay assistance if needed. The pharmacy will ship the medication to your doorstep. Reach out to Rightway whenever you have questions or need help finding lower-cost options.

Manage your prescription.
Check your order status and schedule refills through the specialty pharmacy’s website or app. If you have any trouble getting your medication, contact Rightway—we'll get to the bottom of it.
Your most common questions, answered.
What is a specialty medication?
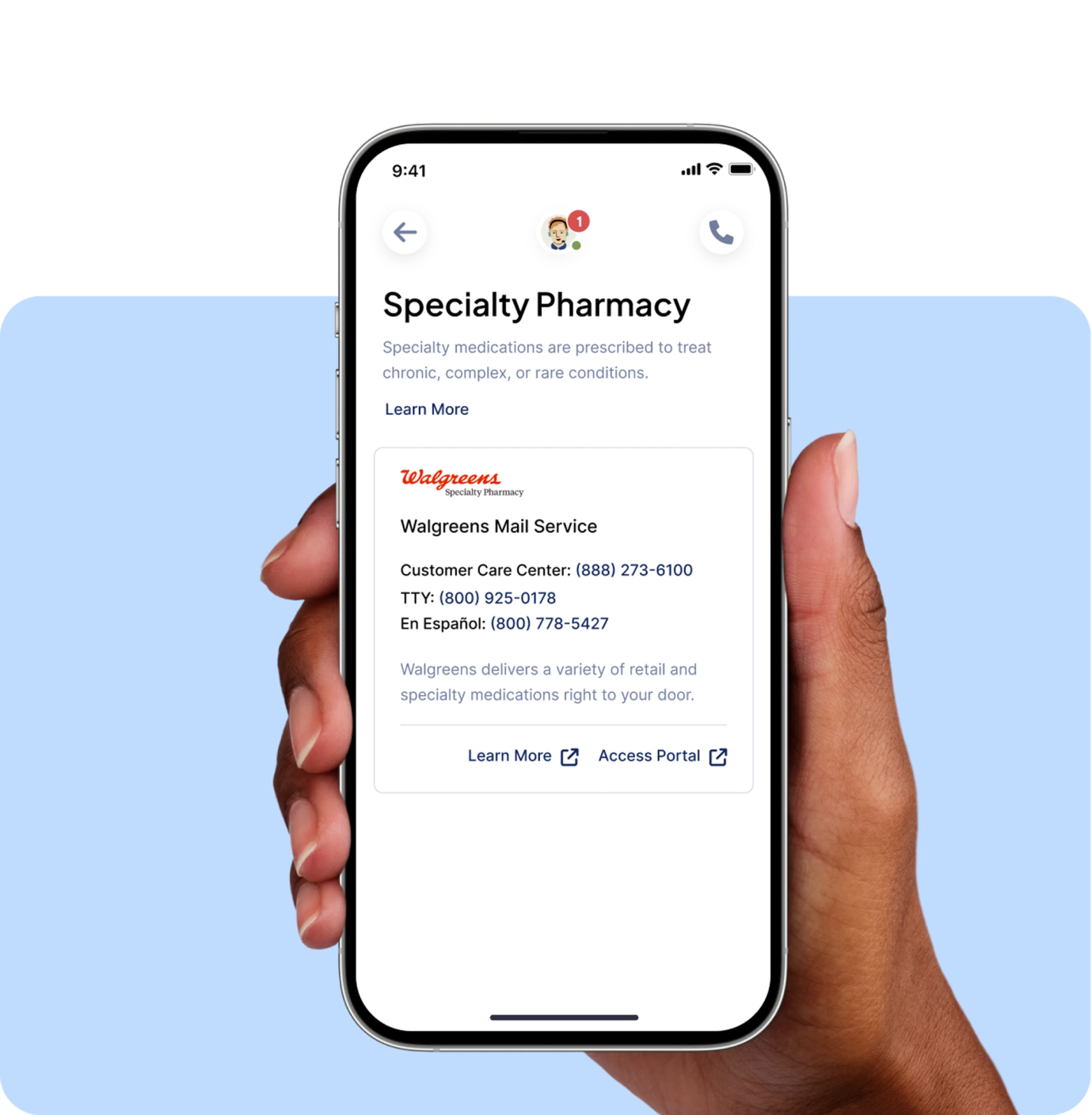
Specialty medications are oral or injectable medications used to treat complex health conditions. These medications may be expensive, require extra attention from your healthcare team, or need special storage. Many specialty medications cannot be filled at traditional pharmacies. Rightway will let you know which specialty pharmacy partner can fill your medication. Our specialty pharmacy team is here to answer any questions about our partners.
How do I fill a specialty medication with Rightway?
A Rightway pharmacist is ready to assist you with all your specialty medication needs. Most specialty medications require your doctor to submit a prior authorization for approval. The Rightway specialty pharmacy team can help by contacting your doctor to start this process. If you are new to Rightway, this approval may have carried over from your previous plan.
You may check the status of your prior authorization request in the medicine cabinet using the Rightway app. You should also ensure your contact information is up-to-date in the app so we can reach you with important updates about your medication.
What is prior authorization?
Prior authorization is when your doctor needs approval before certain medications can be filled using your pharmacy benefits. Your doctor must submit a prior authorization request for Rightway to review and approve. We will inform your doctor once the prior authorization has been approved.
What happens after I receive prior authorization approval?
Once your medication is approved, your doctor will send the prescription to your specialty pharmacy. After receiving your prescription, the pharmacy will contact you.


Have a question? Our pharmacy team has you covered.
Our pharmacy experts are ready to answer your questions and take action for you.